Why
Eye health is particularly important for Autistic people as they are more likely to experience conditions like refractive errors (vision correction needs), strabismus (crossed eyes), and amblyopia (lazy eye).
Autistic people often experience barriers in accessing healthcare, including sensory sensitivities, communication differences and a lack of understanding from providers. This can make accessing eye care stressful and lead to unmet needs. This research aims to identify and address these challenges by working with Autistic people, their families and eye care professionals to make services more accessible, inclusive and affirming, ultimately improving health outcomes and experiences.
What are the eye care experiences of Autistic adults and children?
What are the experiences of eye care professionals in providing services to Autistic people?
How can eye care professionals provide more accessible, inclusive and affirming services for Autistic people?
The research
Study one
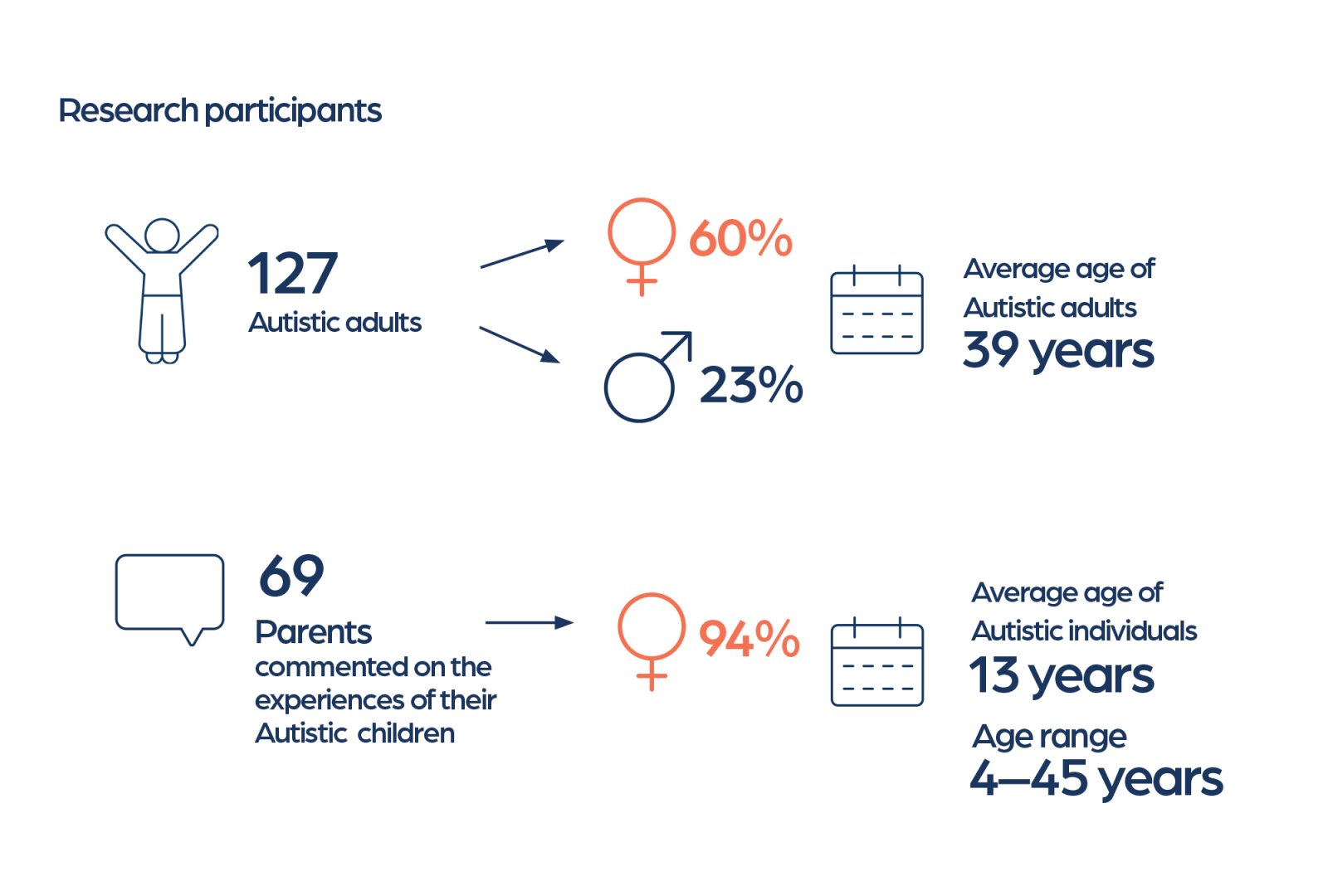
A survey was used to explore the experiences of 127 Autistic adults and 69 parents of Autistic children across Australia and Aotearoa New Zealand.
Study two
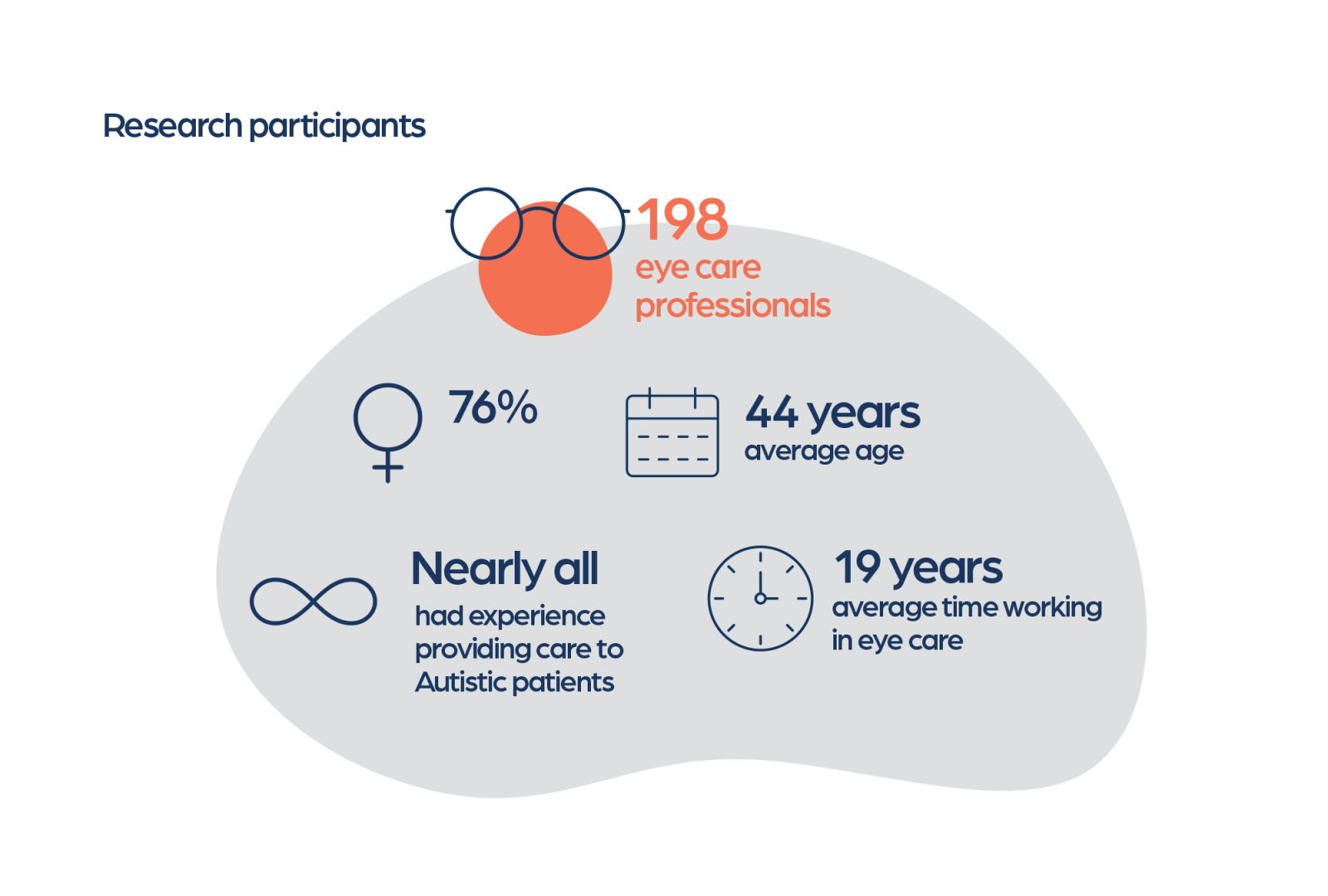
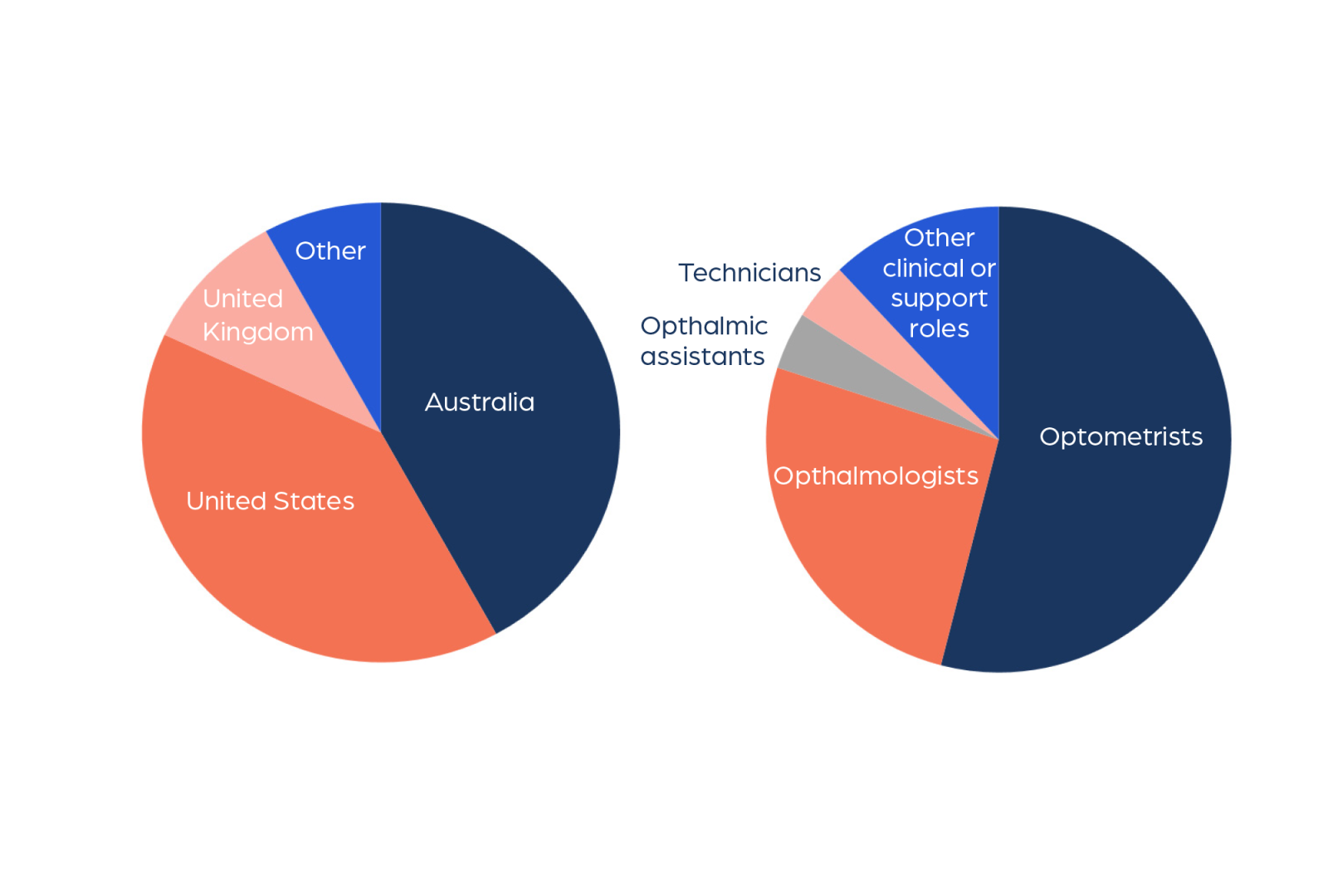
A survey was used to explore the knowledge, confidence and training needs of 198 eye care professionals internationally.
What we learnt
Study one
Top 10 barriers to accessible eye care
Autistic adults
- Sensory sensitivities during eye exams
- Anxiety or stress during eye exams
- Uncomfortable sensory environment when accessing eye care services
- Pressure to make quick decisions (e.g. selecting frames)
- Financial costs
- Multiple staff interactions causing anxiety
- Assessing level of vision during an eye exam
- Remaining still during an eye exam
- Understanding instructions from staff during eye exams
- Scheduling appointments
Parents of Autistic children
- Anxiety or stress during eye exams
- Sensory sensitivities during eye exams
- Understanding instructions from staff during eye exams
- Fear or stress with eye drops
- Communicating with staff
- Lack of understanding of specific needs (e.g. autism)
- Remaining still during an eye exam
- Uncomfortable sensory environment when accessing eye care services
- Multiple staff interactions causing anxiety
- Assessing level of vision during an eye exam
Top 10 supports to make eye care more accessible
Autistic adults
- Eye care staff with knowledge and understanding of autism
- A calm and reassuring environment
- Adjustments to the sensory environment
- Digital reminders and instructions
- Clear and straight forward instructions
- Verbal explanations supported by visual materials
- Plain language communication
- Information provided in advance about what to expect
- Flexible and easy appointment scheduling
- Communication tailored to individual preferences
Parents of Autistic children
- Eye care staff with knowledge and understanding of autism
- A calm and reassuring environment
- Clear and straight forward instructions
- Communication tailored to individual preferences
- Minimising waiting times
- Visual aid
- Adjustments to the sensory environment
- Plain language communication
- Information provided in advance about what to expect
- Opportunities to take breaks
Through thematic analysis of over 600 comments, three key themes were developed.

Theme 1: It all comes down to how they interact with you
Participants described how the quality of interpersonal interactions, particularly communication style, pacing, clarity, and understanding of autism, influenced their overall experiences of eye care. These interactions often determined whether the experience felt supportive and accessible or confusing and distressing.
Theme 2: The experience is too much
Many participants found the clinical environment and procedures overwhelming.

Theme 3: Financial barriers put eye care out of reach
Autistic adults described the cost of eye care, particularly prescription glasses and specialist appointments, as a significant barrier to accessing services.
Study two
Survey results highlighted both strengths and gaps in how eye care professionals support Autistic patients. While many reported confidence in their ability to provide care, most had received little or no formal autism training.
- 61% had a personal or professional connection to autism.
- Autism knowledge was generally high but mostly gained informally; only 14% had formal training.
- Confidence in supporting Autistic patients was moderately high.
- Attitudes toward disability were broadly positive.
- Professionals who saw Autistic patients more often showed greater confidence and more positive attitudes. Other factors (country, connection to autism, years of experience) were not predictive.
- No variables significantly predicted autism knowledge, possibly due to measurement limitations.
Professionals shared open-text reflections on their experiences providing eye care to Autistic patients. These were analysed thematically and grouped into three key areas:
1. Challenges
- Difficulty navigating communication differences
- Managing sensory discomfort and anxiety during exams
- Time pressures and inflexible appointment structures
- Lack of autism-specific training or guidance.
2. Supports
- Using calm, direct, and patient communication
- Offering breaks, reducing environmental stimulation, and adapting tests
- Providing choice and explaining procedures in advance
- Spreading appointments across multiple visits where possible
- Using preparation strategies like visual schedules, photos, or pre-appointment information to help Autistic patients know what to expect.
3. Training and support needs
- Practical, autism-specific training co-developed with Autistic people
- Real-world examples of how to adapt assessments
- System-level support, such as longer appointment times or funding for adjustments.
Publications
Edwards C., Love A.M., Cai R.Y., Constable P., Love D.C., Parmar K., Gowen E., & Gibbs V. (2025). Understanding eye care access for autistic adults and families: A convergent mixed-methods study. Autism.
Edwards C., Love A.M., Cai R.Y., Constable P., Love D.C., Parmar K., Gowen E., & Gibbs V. (2025). Autism in eye care: A mixed-methods study of professional knowledge, confidence and clinical experience. Ophthalmic and Physiological Optics.
Media
Link Magazine: Making eye care more autism friendly (December 2025 – January 2026)
Optometry Australia: Making eye care more inclusive for autistic Australians (1 December 2025)
Making a difference
Based on the findings from both studies, there are clear and practical steps that can be taken to improve access to eye care for Autistic people.
Make eye care environments accessible: Adjust for sensory and communication needs with quieter times, clear language, flexible pacing and information in advance to reduce anxiety and discomfort.
Provide practical, autism-informed training: Co-designed with Autistic people, focusing on real-world communication, rapport-building and adapting tests for adults and children.
Partner to embed inclusive practice: Aspect Autism Friendly to work with providers and shopping centres to pilot autism-friendly models, reduce sensory barriers and integrate inclusive care into everyday service delivery.
Research team
This project is led by experts in autism research and eye care, including:
- Dr Chris Edwards: Adjunct Research Fellow - Griffith University and Research Fellow – Aspect Research Centre for Autism Practice (ARCAP)
- Dr Abbey Love: Research Fellow – ARCAP, Assistant Research Professor – Ball State University
- Dr Ru Ying Cai: Research Fellow – ARCAP
- Dr Paul Constable: Senior Lecturer – Flinders University
- Dr Daniel Love: Assistant Professor Ophthalmology – University of Cincinnati, College of Medicine
- Dr Vicki Gibbs: Head of Research – ARCAP
- Dr Ketan Parmar: Lecturer – The University of Manchester
- Dr Emma Gowen: Senior Lecturer – The University of Manchester
Started
2024
Ends
2025
Funding
Aspect (Autism Spectrum Australia)